Shoes or Achilles Tendonitis: How Rigidity Reduces Tendon Load
Achilles tendinopathy often presents as pain at the back of the heel, especially first thing in the morning or after sitting. Stiffness may ease once you start moving, but the discomfort often returns and tendonitis can persist over time.
Many people switch into softer, more cushioned shoes or add inserts, hoping extra comfort will solve the problem. That approach frequently falls short because excessive softness can increase stress on the Achilles tendon during walking. A shoe’s ability to control motion and resist bending directly affects the load on your tendon.
Achilles tendonitis, also known as Achilles tendinopathy, develops when repeated load exceeds what the Achilles tendon can tolerate.
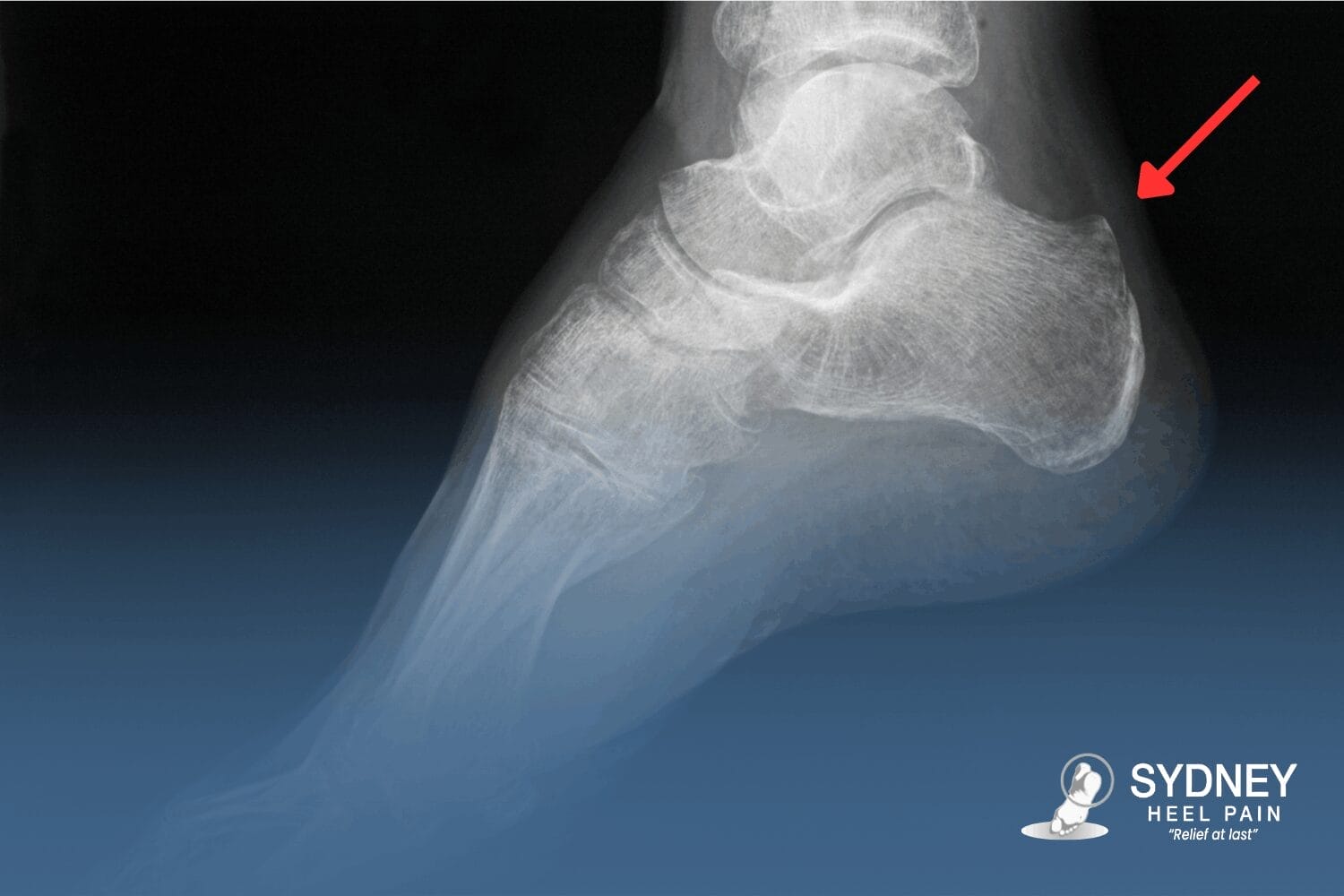
Running, sport, long hours on your feet, and sudden footwear changes often trigger symptoms. Pain is felt at the back of the heel where the Achilles tendon inserts into the heel bone and often intensifies with the first steps after rest or during push-off while walking.
Common triggers include:
- Abrupt increases in training volume.
- Sports involving sprinting, jumping, or rapid direction changes.
- Long periods of standing or walking on hard surfaces.
- Switching into flatter, softer, or more flexible shoes.
Management focuses on unloading rather than cushioning. Reducing shoe bend, increasing heel drop, and limiting excessive motion helps lower strain on the Achilles tendon during walking.
Shoes that increase strain often have these characteristics:
- Very soft cushioning that allows the heel to sink and increases calf demand.
- High flexibility that raises forefoot motion and tendon load.
- Flat shoes that lower heel height and increase stress through the heel bone and Achilles.
Features to Look for in Shoes to Wear with Achiles Tendonitis
The best Achilles tendonitis shoes reduce pull on the Achilles tendon by controlling heel motion and limiting shoe bend. The sections below explain how each feature affects load through the heel and Achilles tendon during daily wear.
Firm, Supportive Heel Counter
A heel counter is the structured section that wraps around the back of your heel and stabilises it as you're walking.
A firm counter limits twisting and side-to-side movement at the back of the heel, which reduces unwanted motion and lowers strain on the Achilles tendon as the foot loads and unloads. This structure pairs well with a firm orthotic, where prescribed, because both work together to control heel motion and reduce Achilles tendon load rather than relying on soft cushioning.
Slight Heel Elevation Without Being “High Heels”
A very soft or overly cushioned shoe can feel comfortable at first but often allows the heel to sink and move excessively under load.
That instability increases strain on the Achilles tendon by forcing it to control motion rather than simply transmit force. A structured midsole provides support and controlled cushion, which reduces unwanted movement and lowers load on the Achilles during walking and standing.
Good Arch Support to Help Unload the Heel
Appropriate arch support helps control how force moves through the foot and ankle, which reduces load through the plantar tissues and the Achilles tendon.
By limiting excessive collapse, support decreases stress at the heel and along the tendon where it inserts into the heel bone. When clinically indicated, Sydney Heel Pain Clinic designs firm custom orthotic devices to unload irritated tissue rather than cushion it, with a 48-hour turnaround to keep treatment moving.
Shoes to Be Cautious With if You have Achilles Tendonitis
Some shoe types increase load through the Achilles tendon by allowing excessive movement at the heel. That movement raises tensile force through the tendon during walking. Repeated loading can aggravate Achilles tendonitis, especially when the calf is tight.
Be careful about wearing:
- Very flat, floppy casual shoes or thongs with thin soles and no heel counter, which let the heel roll and twist and increase strain through the Achilles tendon.
- Extremely soft, heavily cushioned trainers and some running shoe designs that compress under body weight, delay stabilisation, and allow excessive rearfoot motion.
- Minimalist shoes or “barefoot” styles with a very low heel-to-toe drop, introduced suddenly without a transition, which can significantly increase load through the Achilles and calf.
- Flexible slip-on shoes that bend easily through the heel and midfoot, offering little resistance to rearfoot movement during daily wear.
What to Expect if Your Achilles Pain has not Settled
At the first visit, the assessment focuses on understanding what’s driving the excessive force on your Achilles tendon and how to remove it. This includes a review of what you’ve already tried and a biomechanical examination of the foot and ankle, calf, and heel, with gait assessment where indicated.
You can expect:
- A clear mechanical explanation of what’s contributing to symptoms, including how load is moving through the Achilles tendon and surrounding structures.
- Context around past care, including why stretches, inserts, or injections may not have changed symptoms.
- Footwear guidance focused on how your current shoe choices may be influencing ongoing irritation.
Next steps are discussed so you know what to expect:
- A load-based plan that may include footwear changes aimed at reducing irritation rather than masking it.
- Structured lengthening to reduce pull through the Achilles, instead of early strengthening.
- Shockwave therapy is considered for chronic or resistant cases, used alongside footwear changes rather than as a stand-alone option.
When to Seek Professional Help for Your Achilles
Seek professional help when symptoms indicate possible tendon damage or fail to improve with short-term activity reduction. Early assessment helps identify serious injury and reduces the risk of delayed healing.
Seek urgent medical care if you experience:
- A sudden “pop” or “snap” is felt in the calf or heel.
- Immediate severe pain with rapid swelling.
- Inability to bear weight or push off the foot.
- Visible deformity, including a gap or marked change in tendon shape.
Book an appointment if you notice:
- A painful Achilles that persists beyond 10 to 14 days despite rest.
- Ongoing stiffness or swelling, especially on first movement.
- Functional limitation affecting walking, work, or sport.
- Recurrent symptoms that settle briefly then return.
If you’re experiencing any of the signs above, contact Sydney Heel Pain Clinic or book an appointment with a podiatrist.
Shoes for Achilles Tendonitis FAQs
How is Achilles tendonitis different from an Achilles tendon tear or rupture?
Achilles tendonitis develops gradually. The tendon remains intact but becomes overloaded, leading to stiffness and pain with or after activity.
A tear or rupture follows a sudden event. People often report a pop or snap, rapid pain, loss of push-off strength, and difficulty walking, which needs urgent treatment.
Can Achilles tendonitis improve without using custom orthotics?
Yes, some cases settle with load reduction, footwear adjustments, and activity modification. Early guidance can be enough when symptoms are mild and mechanics are favourable.
Orthotics become more relevant when foot mechanics continue to re-load the tendon despite these changes.
Does being flat-footed or having high arches increase Achilles risk?
Both flat feet and high arches can change how load travels through the tendon. The risk relates to movement patterns rather than the label itself. Assessment focuses on mechanics under load, not foot shape alone.
Can standing all day at work contribute to ongoing Achilles pain?
Yes, prolonged standing keeps the tendon under continuous low-grade load. Symptoms can build without obvious spikes in activity. Hard floors and unsupportive footwear can compound this effect.
Does body weight or recent weight gain affect Achilles load?
Higher body weight increases force through the tendon with every step. Load rises even during routine walking. Recent weight gain combined with activity changes can trigger symptoms more easily.