Plantar Fasciitis Treatment IN Sydney CBD
(and our other clinics)
Chronic plantar fasciitis is a load-based mechanical condition that often fails to respond to stretching, rest, or generalised advice. The tissue is being irritated for a reason — and that reason must be identified.
At Sydney Heel Pain Clinic, we perform biomechanical assessment and mechanical fault isolation in patients with persistent heel pain, particularly plantar fasciitis. From our Sydney CBD clinic (and our other locations), we manage new cases and complex cases that have not responded to conventional podiatry, passive therapy, or symptomatic interventions. Every assessment is structured around three questions:
- Where is the mechanical overload occurring?
- What specific movement, postural habit, footwear, or structural issue is driving it?
- How do we remove the barrier to tissue recovery?
This is not a generic protocol-based approach to treatment. Each case is assessed using:
- Digital gait analysis to measure real-time loading and force transfer
- 3D foot scanning to identify abnormal structure or arch mechanics
- Functional load testing of the fascia, calf complex, and surrounding structures
- Detailed history to identify movement patterns and habits preventing resolution
Many patients presenting for plantar fasciitis treatment in Sydney CBD have previously received orthotics, cortisone injections, or generic exercise programs with minimal change. In most of those cases, the mechanical driver was never addressed.
If the fascia continues to be irritated under load, it will not resolve — regardless of rest, taping, or soft tissue release.
Treatment Methods and clinical services
Shockwave Therapy for Chronic Plantar Fasciitis and Tendinopathy
Shockwave therapy is a non-invasive, evidence-based modality used in the management of chronic plantar fasciitis, tendinopathies, and mechanically induced soft tissue overload. This treatment delivers focused acoustic energy to the affected tissue, initiating neovascularisation and disrupting persistent nociceptive signalling. It accelerates tissue regeneration without the need for corticosteroid injections, surgical intervention, or extended immobilisation.

Footwear Prescription Based on Biomechanical Load
Footwear is prescribed following gait analysis and structural evaluation, with recommendations tailored to the patient's specific loading mechanics. Selection is driven by measurable force patterns and joint stress, not aesthetics or brand marketing. In many cases, correcting load distribution through appropriate footwear alone results in significant symptom reduction.
3D-Printed Orthotics for Targeted Load Correction
When clinically indicated, custom orthotics are prescribed based on detailed digital scans of the patient’s foot structure and gait profile. Using advanced 3D-printing technology, each device is fabricated to optimise joint alignment and redistribute mechanical load according to the patient’s specific pathology. These are precision-manufactured medical-grade devices — not prefabricated insoles — and are integral in managing complex loading faults that contribute to chronic plantar fasciitis.
Stretching and Load Management Protocols
Targeted stretching and progressive load modulation are prescribed to address biomechanical restrictions and soft tissue dysfunction contributing to plantar fasciitis. Calf complex tightness and fascial retraction are frequently identified as upstream drivers of pathological tension through the plantar fascia. These protocols are critical in restoring tolerance to tensile and compressive forces and are often used in conjunction with orthotic therapy or shockwave intervention.
Clinical Background
Dr Karl is a podiatrist with over two decades of clinical experience in the diagnosis and management of mechanical foot and heel pain. Graduating with honours from the University of Salford (Manchester) in 1998, his career has been defined by a biomechanical approach to lower limb pathology, with a particular focus on chronic plantar fasciitis and arch-related dysfunction.
Dr Lockett has contributed to professional education through guest lecturing at the University of Western Sydney on topics relating to mechanical dysfunction and load-induced foot pain. Since 2020, he has held the position of consulting podiatrist to the Sydney Opera House, where he provides specialised care in a complex occupational setting.
He is frequently consulted by patients across Sydney, regional New South Wales, interstate, and internationally — particularly in cases where prior interventions have not achieved resolution.
This is not a generic protocol-based approach to treatment. Each case is assessed using:
- Digital gait analysis to measure real-time loading and force transfer
- 3D foot scanning to identify abnormal structure or arch mechanics
- Functional load testing of the fascia, calf complex, and surrounding structures
- Detailed history to identify movement patterns and habits preventing resolution
Many patients presenting for plantar fasciitis treatment in Sydney CBD have previously received orthotics, cortisone injections, or generic exercise programs with minimal change. In most of those cases, the mechanical driver was never addressed.
If the fascia continues to be irritated under load, it will not resolve — regardless of rest, taping, or soft tissue release.
This Breakthrough ‘HeelWave’ Therapy Fully Resolves Plantar Fasciitis Forever In Just 42 Days (Pain Free After First Appointment – Guaranteed!).
Are you suffering from heel pain? It might be caused by plantar fasciitis. Our sports injury clinic specialises in the diagnosis and treatment of plantar fasciitis.
What is Plantar Fasciitis?
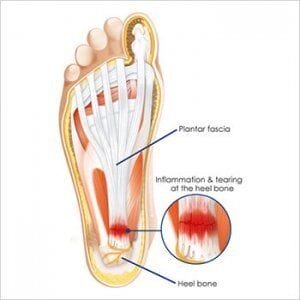
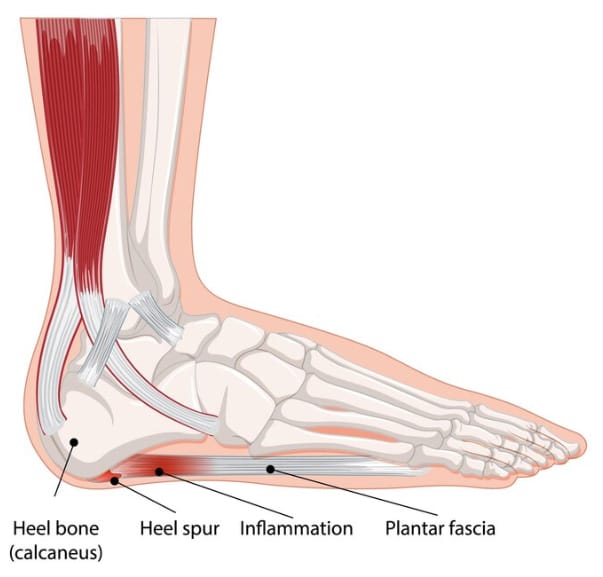
Plantar fasciitis is a painful inflammatory heel condition affecting the large ligament-type structure in the base of the foot that can cause arch pain and heel pain. The plantar fascia can become thick and inflamed due to the irritation at its attachment, at the base of the heel bone. In some patients, small tears can develop and these people suffer from acute pain that can be excruciating. Sometimes, on x-ray, heel spurs (bone spurs) can be seen, but these are not usually the cause of the patient’s heel pain.
It should be noted that “heel spurs” is a misleading diagnosis that has been used by podiatrists and doctors for many years. More and more practitioners today are open to the fact that heel spurs are not the problem and that these bone spurs don’t cause pain. Instead, the source of pain is the inflammation within the plantar fascia surrounding the spur itself.
What Does Plantar Fasciitis Feel Like?
Patients with plantar fasciitis usually feel pain under the ball of the heel and it can represent a stone bruise sensation. Arch pain is less common but is also a key symptom of the condition. The heel pain is common first thing in the morning when climbing out of bed and after periods of rest, such as driving or being seated. The pain in the heel can be erratic and often, there are pain-free periods when the person feels like they are healing. If there is a very sudden onset of pain, as opposed to a gradual onset, this may be due to tearing of the plantar fascia.
These classic signs are frequently reported by patients attending for plantar fasciitis treatment in Sydney.
Correct Diagnosis for Plantar Fasciitis
It is important that the podiatrist differentiates between regular plantar fasciitis, and plantar fascia tearing as the treatment is different. Your podiatrist will also be able to exclude the possibility of a stress fracture, which sometimes leads to similar symptoms. Ultrasound imaging may be necessary to accurately diagnose the cause of the patient’s heel pain.
Correct diagnosis is essential in delivering effective plantar fasciitis treatment, particularly in more complex or chronic cases seen in our Sydney CBD clinic.
The Stages of Plantar Fasciitis
Initial Stages of Plantar Fasciitis
- Initially, these heel pain patients may feel a dull ache in the base of the heel. There may be an awareness of a problem in the afternoons, or after they have been weight-bearing for long periods of time. It is possible that they feel some pulling in the plantar fascia, which they describe as a tightness in the arch or the sole of the foot.
- Early treatment or intervention at this stage is crucial and may inhibit the development of a more chronic heel pain condition. Unfortunately, many patients ignore the early symptoms, presuming or hoping that the tightness or the dull ache in the heel will settle down and dissipate. In some people, this is the case, but others can develop severe heel pain and/or chronic P.F.

- As sports podiatrists, the typical symptoms that we hear in these early stages, are the feeling of a pebble in the shoe or a stone bruise sensation. Patients with mild P.F sometimes inform us that they felt like they had stepped on a small pebble or stone.
- In these early stages that we describe above, the condition does not always induce heel pain throughout the daytime. The symptoms may only be present in the morning when getting out of bed and can be very sporadic. Some patients are asymptomatic for a day or two only to find the pain returning.
- In the early stages, there can also be some heel pain in the morning when the foot hits the floor, but this is usually mild and is often little more than a feeling of tightness.

Chronic Plantar Fasciitis
When the condition is fully developed, the symptoms of plantar fasciitis heel pain are more acute. The condition will become chronic if the strain on the plantar fascia goes on for long enough and remains untreated.
The pain in the heel is more consistent and patients will usually report pain, not just stiffness, each morning when hopping out of bed. Most patients hobble for at least 5 minutes after getting out of bed due to extreme plantar fasciitis heel pain.
The pain in the heel usually subsides within 15 minutes and patients are usually more comfortable after taking a hot shower. Walking throughout the day isn’t always a problem as the inflammatory change in the plantar fascia is less consistent and the heel pain isn’t always present.
However, mid-afternoon, after several thousand steps the foot fatigues, and the heel pain returns. Patients will sometimes report pain when getting out of their car after a drive home from work. They hobble again for the first few minutes and find some relief after walking a short distance.
Podiatrists are often informed by their patients that they also limp when they stand up after being seated for dinner in the evenings or after sitting on the couch watching television. An ultrasound report will often show thickening of the plantar fascia, due to inflammatory change.
Severe Plantar Fasciitis
If the condition comes on very quickly, during a one-off event or during a particular day/activity then the pain can feel severe/acute. Alternatively, chronic plantar fasciitis left untreated can lead to the same state.
Acute Inflammation
In these cases, the strain on the plantar fascia has been so great and so repetitive that acute inflammation develops as does extreme pain. Patients with severe P.F will usually describe to the sports podiatrist an extreme level of pain that is present for most of the day. These patients will experience throbbing when sitting or lying down and are starting to feel the psychological effects of having a condition that is both chronic and acute.

Often described as “excruciating” or “relentless”, heel pain plantar fasciitis patients experience symptoms that affect their daily lives, as they stop exercising and are often struggling to walk during day-to-day movements.
Some patients with severe P.F have developed deep surface or laminar tears in the fascia. As sports podiatrists, we arrange ultrasound scans, to help confirm or exclude torn fascia. X-rays are less helpful in the case of this soft tissue injury.

Who Suffers From Plantar Fasciitis Heel Pain?
Plantar fasciitis can affect men and women equally, but there is a trend in terms of the age of the patients that we treat. Fewer people younger than 30 years of age develop the condition, and the majority of patients are over 60. In between those ages, there is a large percentage of male and female patients in their 40’s and 50’s.
Sedentary people who haven’t exercised for some time, who enter a get fit health program of sorts, and those who join a boot camp, will often develop pain in the heel or Achilles tendon, namely plantar fasciitis, Achilles Tendonitis, or Bursitis. Treating the Achilles tendon is crucial in these cases to prevent further complications.
Occasionally we see juvenile-onset P.F which affects children who are engaged in sport and physical activity. It is important that we differentiate between other heel pain conditions such as Severs disease and Achilles Tendonitis
Our sports podiatrists have extensive experience in these conditions and can determine which one your child has, by carrying out a careful physical examination. We will refer for x-ray or ultrasound scans if we deem them necessary.
Multifactorial Causes
CAUSES OF PLANTAR FASCIITIS
There is no single cause of plantar fasciitis. The cause is multifactorial, as is the plantar fasciitis treatment. Ultimately, there is an increased load on the plantar fascia which causes it to become pathological. Tight calf muscles and soft shoes are a big problem, as are flat feet and an increase in body weight. Biomechanical issues leading to poor foot function can also trigger the condition. Patients who suddenly increase the amount or frequency of sporting activity/exercise are also at risk.
We often hear patients saying, “I was looking to get fit after Christmas and was training several times a week, and then my heel became extremely painful…”
Common Mechanical Factors in Sydney Plantar Fasciitis Cases
Footwear and Plantar Fasciitis
Commonly, people with plantar fasciitis have been using flat, flexible, and less supportive shoes. The lack of support is stressful on the plantar fascia and the heel bone, especially for those people with a weaker foot type. If these patients use the softer shoes for long enough periods, or as the main shoe, the stress can lead to P.F or other types of heel pain. In these circumstances, it is essential that the patient has their foot type and shoes assessed. This will help the plantar fasciitis treatment. Interestingly, higher-heeled shoes for women are not the cause of plantar fasciitis, although these shoes do cause tightness in the calf muscles. Most women report, “my heel pain feels better in a high heel”.
High Arches
People with higher arches receive less support from shoes and their liners, as there is less contact through the sole/arch area. The plantar fascia runs through this arch area and can become taught and strained. Functional running shoes and hiking shoes still lack the arch support that some feet need. The lack of support and the tightness can lead to heel pain and the development of the condition.
Flat Feet
The flat foot (pes planus) is often caused by weak ligaments (ligament laxity). The plantar fascia works harder, along with other muscles and tendons, to compensate for this inherent weakness. The increased load can lead to P.F or heel pain in general if the increased load is sufficient to cause strain, tearing, and inflammation.
Overstretching
The most common calf stretches place a certain amount of strain through the sole of the foot and therefore, the plantar fascia. Plantar fasciitis can come about when the patient stretches too much, or too hard. Some patients go through a rehab period following an injury or surgery and will develop plantar fasciitis due to the stretching technique they used. This is not to say that calf stretching should be avoided, but more so that technique is important.
Bodyweight and Plantar Fasciitis
A large percentage of patients that we treat with plantar fasciitis are carrying more body weight than they want to or are used to. They often report being overweight and are sometimes attempting to shed a few kilos. The increase in body weight adds more load to the feet and hence more strain on the plantar fascia. Furthermore, the increased body mass means that the calf muscles must work harder to push the patient forwards and so these muscles become tight and stiff. As mentioned previously, tight calf muscles pull harder on the heel bone at the Achilles tendon, and will most certainly cause a heel pain condition such as plantar fasciitis or Achilles tendonitis. The irony lies in the fact that these patients are unable to lose weight through their desired walking or other exercise programs as their feet hurt too much. The only way they can lose weight is to engage in non-weight-bearing activities such as swimming.
Treatment Approach for Sydney-Based Patients
For patients based in Sydney Plantar Fasciitis treatment is directed toward biomechanical resolution — not just symptom suppression. The clinical objective is to identify and address the mechanical barrier to tissue recovery, delivering sustained outcomes in cases of plantar fasciitis and other heel-related conditions.
Treatment selection is case-specific. Following diagnostic assessment, Dr Karl Lockett formulates an evidence-based management plan using one or more interventions tailored to the patient's mechanical presentation, symptom chronicity, and functional demands. This may include shockwave therapy, load modification, orthotic prescription, or gait re-training — applied based on measurable dysfunction rather than generic protocol.
PLANTAR FASCIITIS TREATMENT
Our in house treatment objective is to provide a long-term solution to your heel pain condition, and not just quick pain relief. Our sports podiatrists have a wealth of experience in treating plantar fasciitis, as well as all other types of painful heel conditions.
Karl will select an appropriate combination of one or more treatments to suit the severity of your plantar fasciitis and your lifestyle.
Examples of Plantar Fasciitis Treatment (Sydney CBD Clinic)
Some common treatments may include:
- Extracorporeal shockwave therapy with strapping
- Use of an immobilisation boot
- Footwear changes/recommendations with strapping and stretching
- Custom-tailored prescription orthotics (gentle arches) with shockwave therapy.
Our team uses orthotics for plantar fasciitis that are specifically designed as to not push upwards against the plantar fascia. Although going against the grain of the traditional arch support theory (old science) our orthotics unload and support the plantar fascia so that injections and medications are not required, allowing the foot to heal naturally.
You can find out more about our orthotic inserts for plantar fasciitis treatment on our orthotics page or on our blog.
Written by Karl Lockett
Relevant information about plantar fasciitis:
https://www.mayoclinic.org/diseases-conditions/plantar-fasciitis/symptoms-causes/syc-20354846
https://www.health.harvard.edu/newsletter_article/easing_the_pain_of_plantar_fasciitis
https://www.webmd.com/fitness-exercise/understanding-plantar-fasciitis-basics